Blog Post Title: The Power of Stress Management in Boosting Success Rates of Intra Cervical Insemination and IVF
Stress is a common and inevitable part of our lives, and it can have a significant impact on our physical and mental well-being. When trying to conceive, stress can become even more overwhelming as couples navigate the emotional and physical challenges of fertility treatments. Intra Cervical Insemination (ICI) and In Vitro Fertilization (IVF) are two common fertility treatments that have been proven to help many couples achieve their dream of starting a family. However, the success rates of these treatments can be greatly affected by the level of stress a person experiences. In this blog post, we will explore the impact of stress management on ICI and IVF, and how taking care of one’s mental health can increase the chances of a successful pregnancy.
Understanding Intra Cervical Insemination (ICI) and In Vitro Fertilization (IVF)
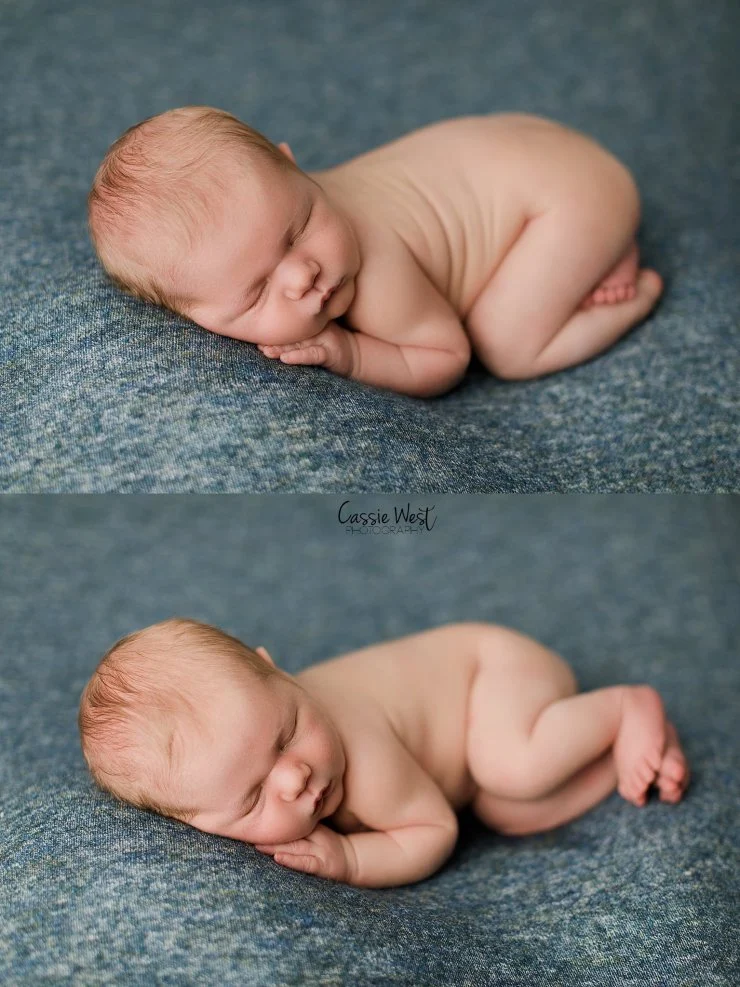
Before delving into the connection between stress management and ICI/IVF, let’s first understand these two fertility treatments. ICI is a procedure where washed and concentrated sperm is placed directly into a woman’s cervix through a catheter. This method is often used for couples with unexplained infertility or mild male factor infertility. On the other hand, IVF involves retrieving eggs from a woman’s ovaries and fertilizing them with sperm in a laboratory. The fertilized eggs are then transferred back into the woman’s uterus, and if successful, the embryo will implant and result in a pregnancy. IVF is commonly used for couples with more severe infertility issues, such as blocked fallopian tubes or severe male factor infertility.
While both ICI and IVF are effective fertility treatments, they can also be emotionally and physically taxing for those going through them. The process of undergoing fertility treatments can be stressful and overwhelming, and this stress can have a significant impact on the outcome of the treatments.
The Connection Between Stress and Fertility
Stress can affect fertility in different ways. Firstly, it can lead to hormonal imbalances, such as an increase in cortisol and adrenaline levels, which can interfere with the production of reproductive hormones. This can disrupt the menstrual cycle and ovulation, making it harder to conceive. Secondly, stress can also cause physical symptoms such as headaches, digestive issues, and fatigue, which can make it more challenging to manage the physical demands of fertility treatments. Lastly, stress can take a toll on one’s mental health, leading to anxiety, depression, and a decrease in overall well-being. These mental health issues can also contribute to the success rates of fertility treatments.
The Impact of Stress on ICI and IVF Success Rates

The Impact of Stress Management on Intra Cervical Insemination and IVF
Studies have shown that stress can significantly impact the success rates of ICI and IVF. One study found that women with higher levels of stress and anxiety had lower pregnancy rates after IVF compared to those with lower stress levels. Another study found that women who participated in a mind-body program to reduce stress before and during IVF treatment had a higher chance of achieving a successful pregnancy. Furthermore, a study on couples undergoing ICI found that those who reported higher levels of stress and anxiety had a lower chance of conceiving compared to those with lower stress levels.
How Stress Management Can Improve the Success Rates of ICI and IVF
The good news is that stress management techniques can help improve the success rates of ICI and IVF. Here are some ways to manage stress during fertility treatments:
1. Prioritize self-care: Self-care is crucial during this time. Take care of yourself by getting enough rest, eating a healthy and balanced diet, and engaging in activities that bring you joy and relaxation.
2. Practice mindfulness: Mindfulness practices such as meditation, yoga, and deep breathing can help reduce stress and promote relaxation.
3. Seek support: Going through fertility treatments can be isolating, but it’s essential to seek support from loved ones or join a support group. Having a strong support system can help reduce stress and make the journey more manageable.
4. Consider therapy: Therapy can be a helpful tool in managing stress and improving mental health during fertility treatments. A therapist can provide coping strategies and support to navigate the challenges of the process.
5. Try acupuncture: Acupuncture has been shown to reduce stress and improve fertility when used in conjunction with ICI or IVF treatments.
In summary, stress management is crucial in improving the success rates of ICI and IVF. Stress can have a significant impact on fertility, and taking care of one’s mental health can significantly increase the chances of a successful pregnancy. If you’re undergoing fertility treatments, make sure to prioritize self-care, practice mindfulness, seek support, consider therapy, and try acupuncture. Remember, a healthy mind and body can greatly contribute to a successful pregnancy.